MJ Chehade, creador de la clínica virtual en un hospital australiano, presenta la experiencia sobre el proyecto Digital Health Hub, impulsado por el Consejo Nacional de Investigación Médica y de Salud de Australia.
El boletín, responde inicialmente a la problemática de la multimorbilidad, es decir cuando los individuos presentan más de una enfermedad crónica diagnosticada. Esto no se relaciona solamente a características de salud sino también a aquellas relacionadas a factores socioeconómicos, culturales, ambientales y de comportamiento.
La Organización Mundial de la Salud (OMS), reconoce los esfuerzos para la creación de modelos complejos de atención que involucren distintas disciplinas de atención sanitaria y social. El boletín recoge diversas experiencias y perspectivas de una comunidad de profesionales de diferentes disciplinas, destacando la importancia de “la agencia del paciente para impulsar la evolución de los servicios de salud” especialmente aquellas estrategias habilitadas digitalmente para la educación del paciente”.

Community-driven progress. Las nuevas prácticas de cuidado de la salud ya no dependen únicamente del personal de salud, ahora existe un mayor acceso a información sanitaria que ha permitido mayor participación de pacientes y sus cuidadores (formales, como personal de enfermería o informales, como familiares).
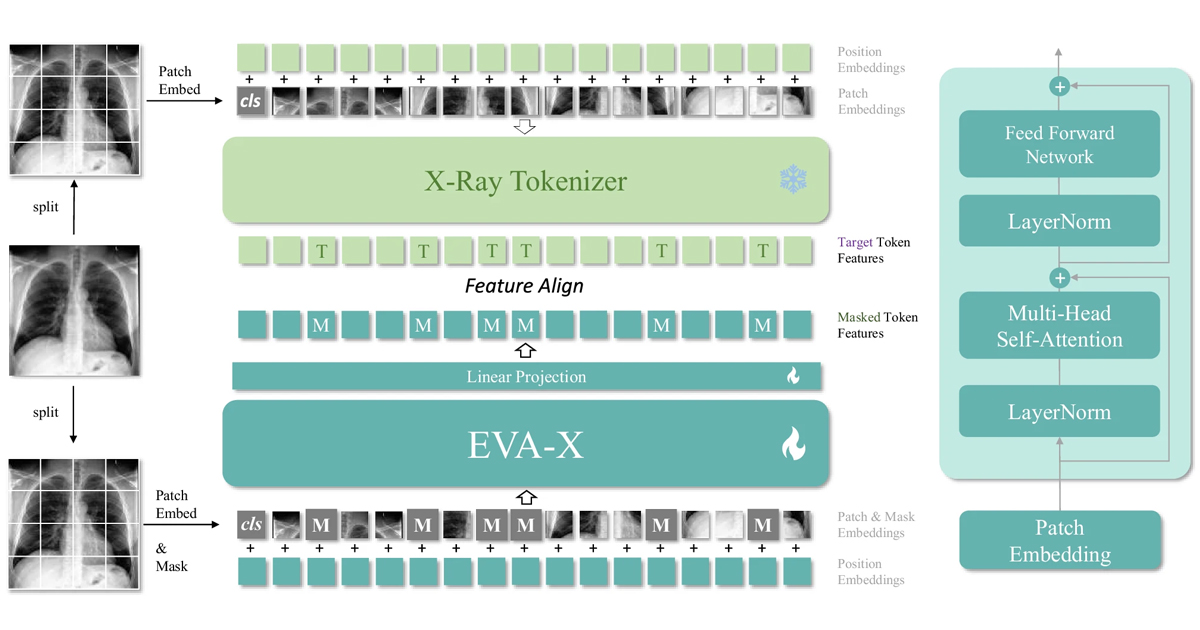
Educación del paciente. In its Report on Human Resources for Health: Workforce 2030, la OMS describe los desafíos para lograr cobertura de salud universal. Uno de ellos es la capacitación del personal de salud, la fuerza laboral facultaría la recopilación y uso del Big Data, por ejemplo, o la Inteligencia artificial aplicada en salud, “la OMS introdujo la digital health como un término amplio para abarcar los servicios de salud prestados electrónicamente (eHealth), incluidas las soluciones de tecnología de salud móvil (mHealth), así como áreas emergentes, como el uso avanzado de las ciencias de la computación para gestionar macrodatos, genómica y sistemas de inteligencia”, explican en el boletín. El desafío consiste en el procesamiento de este tipo de datos recopilados a través de medios digitales.
The proposal of Centers of Digital Health personal, para interpretar la información y lograr una fácil integración de los diversos servicios de salud es una propuesta clave para la resolución de los desafíos que plantea la OMS. “Este centro personalizado es potencialmente una herramienta poderosa que permite a los pacientes tener un mayor control de sus objetivos de salud”, mencionan en el boletín. La existencia de software adaptable para la creación de este tipo de centros digitales que ya son utilizados en sistemas educativos, sería un avance importante para adaptarlos a las necesidades de los servicios sanitarios de cada país.
Among the experiences is the Royal Adelaide Hospital in Australia, where diseñaron una clínica virtual y un centro de digital health para pacientes con un enfoque transdisciplinario: “Se proporcionaron datos de disciplinas clínicas (geriatría, ortopedia, medicina de emergencia, anestesiología, medicina de rehabilitación, medicina general, enfermería, salud afines y farmacia); disciplinas no clínicas (economía de la salud, informática, educación superior, matemáticas, arquitectura y demografía); y grupos de pacientes y consumidores. Utilizamos un enfoque colaborativo y de codiseño para traducir nuestro conocimiento y experiencia en resultados de salud exitosos”.
Para leer el boletín completo, ingresa al siguiente enlace: