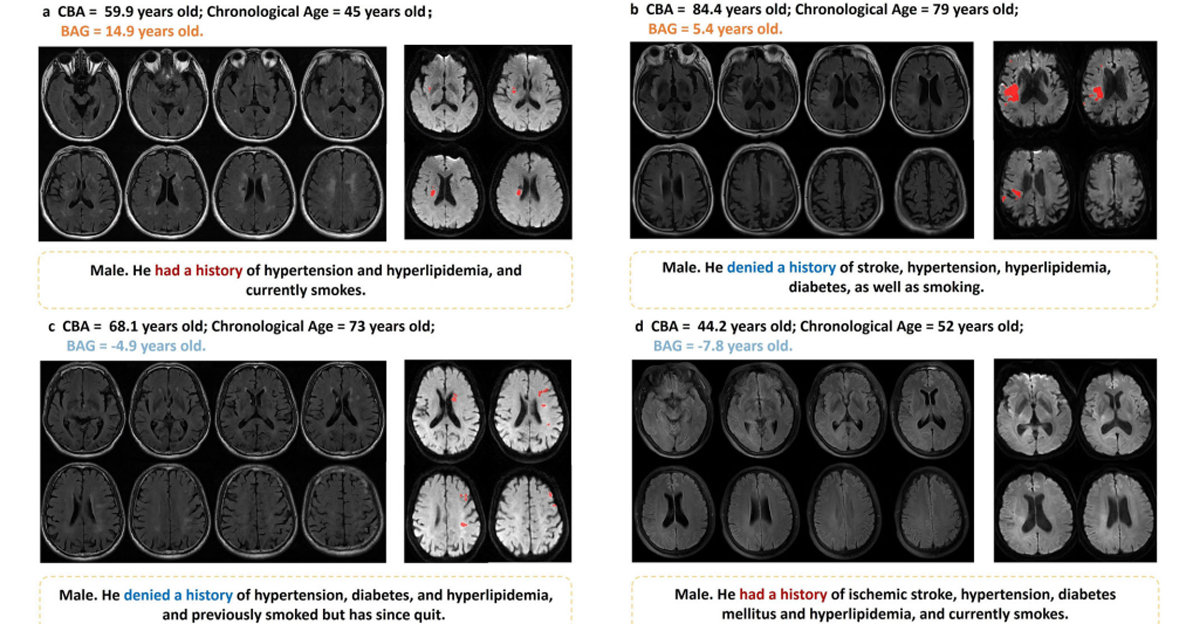
Los puntajes de riesgo se utilizan para tomar decisiones clínicas con mayor información, además la implementación de aprendizaje automático es útil para la identificación de predictores importantes para la creación de puntajes.
Gracias a las puntuaciones de riesgo, los médicos pueden realizar evaluaciones más rápidas sobre el riesgo de un paciente de alcanzar puntajes asociados con predictores claves de riesgo. Por otro lado, el machine learning mejora estos procesos, al contar con herramientas con mayor capacidad para la selección de variables. Un estudio publicado en PLOS Digital Health, realizó una conexión entre herramientas de machine learning (AutoScore) y las herramientas de puntuación de riesgo (ShapleyVIC).
Para el estudio, los autores propusieron un mecanismo de selección de variables ya que conectar ambas herramientas de manera directa podría afectar la interpretabilidad y el rendimiento predictivo. El modelo desarrollado se adapta a puntajes de riesgo y fue integrado a un marco automatizado para el desarrollo del puntaje de riesgo.
El estudio demostró como el método propuesto puede ayudar a que investigadores comprendan las 41 variables candidatas a la predicción de resultados. “Hemos presentado una herramienta útil para apoyar la toma transparente de decisiones de alto riesgo”, explica el estudio.

Esta investigación se enfocó en la muerte prematura o readmisión no planificada después del alta hospitalaria. El de selección de variables, obtuvo 6 variables de 41 candidatos para desarrollar la puntuación de riesgo de un rendimiento aceptable, este tuvo un rendimiento similar al de un modelo de 16 variables basado en machine learning.
“Nuestro trabajo contribuye al énfasis reciente en la interpretabilidad de los modelos de predicción para la toma de decisiones de alto riesgo, proporcionando una solución disciplinada para la evaluación detallada de la importancia variable y el desarrollo transparente de puntuaciones de riesgo clínico parsimoniosas”, explica el artículo.
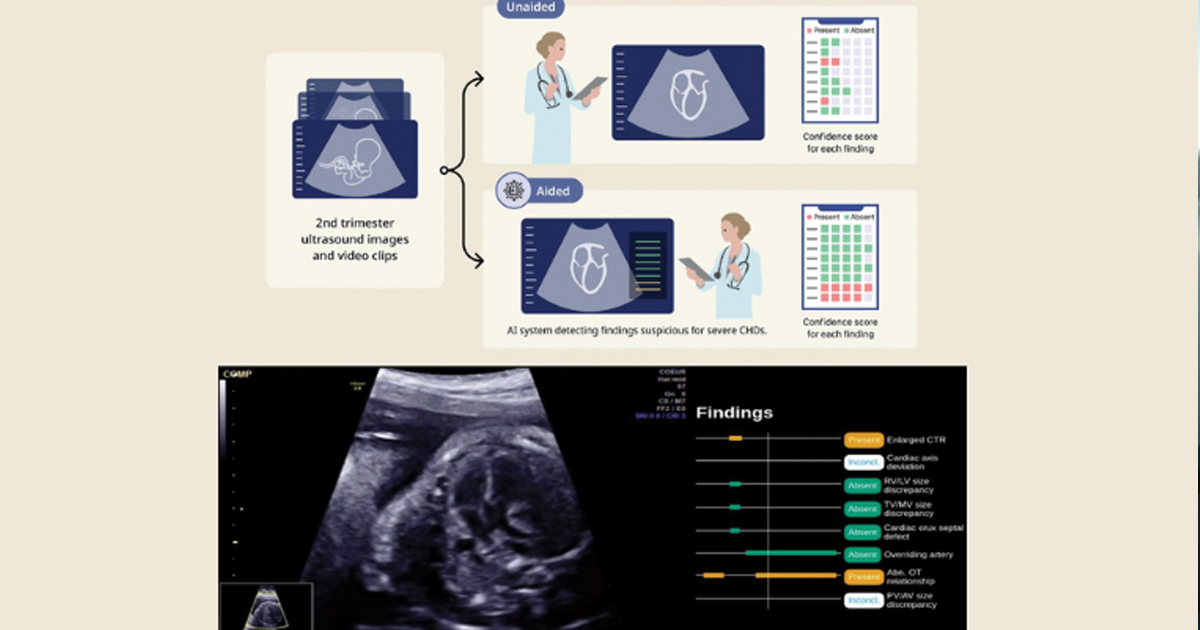
Uno de los modelos utilizados para el estudio, AutoScore, ha sido probado en diversos entornos como para derivar puntuaciones de riesgo en triaje en servicio de urgencias, así como para proporcionar puntuaciones en supervivencia luego de un paro cardíaco extrahospitalarios.
Consulta más detalles sobre ambos modelos y sus resultados leyendo el estudio completo en el siguiente enlace:
https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000062